Pelvic Organ Prolapse (POP) doesn’t only happen to older women, it happens more than you might think.
❗️50% of women of childbearing age will experience some level of Pelvic Organ Prolapse❗️
What is Pelvic Organ Prolapse?
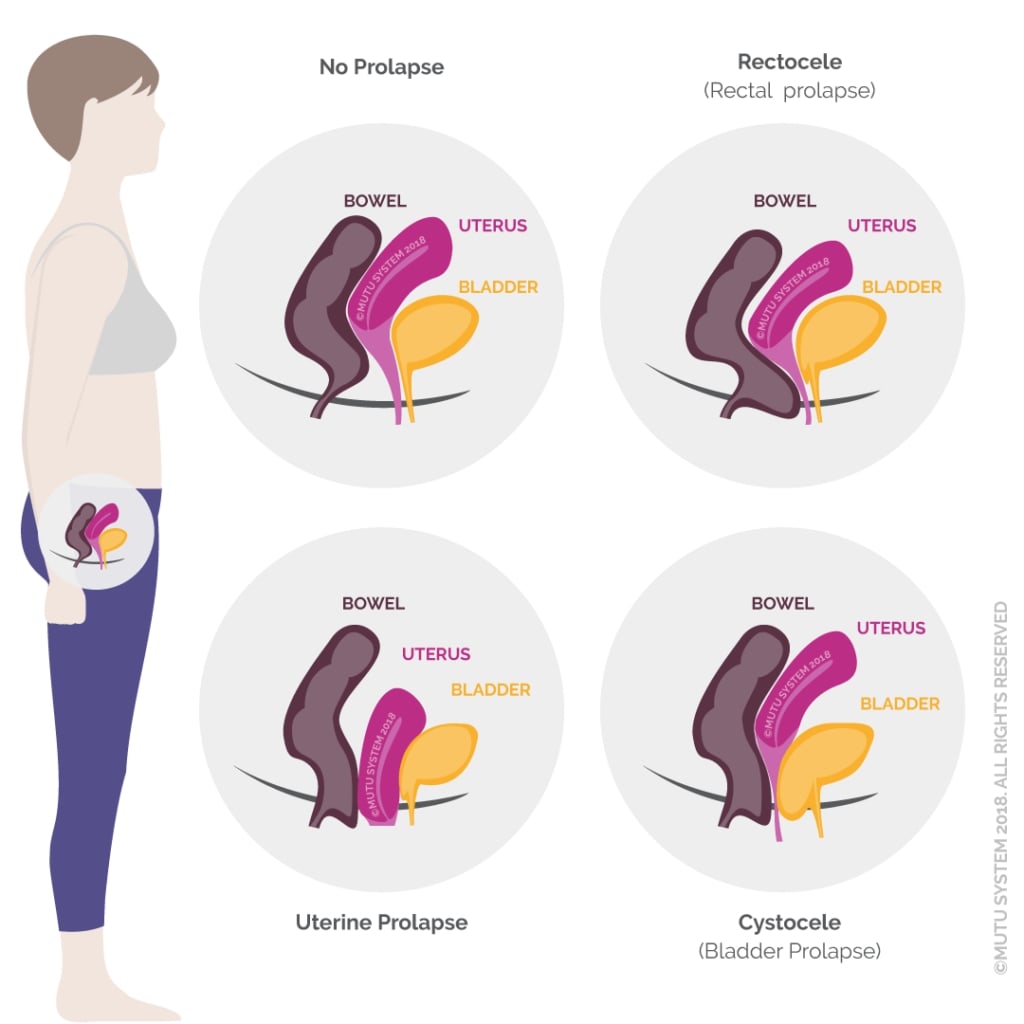
TL;DR? Any kind of prolapse means that one or more organs of your abdomen or pelvis have dropped or shifted position. This can result in discomfort or lack of healthy function.
There are 5 types of pelvic organ prolapse: cystyocele (bladder drops and bulges into the vaginal canal), rectocele (large bowel or rectum bulges into the vaginal wall), enterocele (intestines), vaginal vault (vagina caves in on itself, possibly after uterus is removed-hysterectomy), and uterine (uterus drops).
It is measured in Grades 0-4. 0 is normal or optimal positioning, 1 or 2 may result in mild or moderate symptoms but are unlikely to require surgical intervention, Grade 4 refers to a prolapse that has actually protruded right outside of the body.
Prolapse Symptoms
How do you know if you have it? Each of these 5 types of prolapse has its own symptoms, but in general, symptoms can include:
- Pressure, pain, bulging or fullness in vagina, rectum, or both.
- Feeling like your “insides are falling out” or like you are sitting on a ball.
- Urinary incontinence.
- Urine retention (you have to pee, you just can’t get it to come out).
- Fecal incontinence.
- Constipation.
- Back/abdominal pain.
- Lack of sexual sensation.
- Painful intercourse.
- Can’t keep a tampon in.
It feels pretty horrible and it may be something you don’t feel comfortable talking about, so… Here’s everything you need to know.
What causes pelvic organ prolapse?
Prolapse, Hernia and Diastasis Recti are related conditions in that they are all caused by excessive pressure inside your abdomen and pelvis. The pressure pushes everything away, outwards and downwards.
It’s the job of your core and pelvic floor muscle system to keep this natural pressure contained so that your abdomen and pelvis can function how you want them to. But if alignment or posture has shifted, if you had a prolonged or complicated birth, if you’re getting older or if you’re one of many non-postpartum women who experience pelvic floor dysfunction, the pressure might be ‘off’.

Pregnancy doesn’t cause prolapse and neither does simply a weak pelvic floor. However, there is no question that prolonged labor and pushing, or medical intervention such as forceps or ventouse, may increase the likelihood of prolapse occurring.
What can you do to prevent or relieve symptoms?

Important! A prolapse will not inevitably worsen, so if you are suffering from Grade 1 or 2 symptoms, preventative and healing strategies and changes can prevent your prolapse from escalating.
The solution involves, but is not isolated to, your pelvic floor. Here are some ways you can start to correct the pressure inside your abdomen and pelvis right away and start to reverse the symptoms AND CAUSES of pelvic organ prolapse:
Alignment and pelvic organ prolapse
Alignment means your bio-mechanics, your posture, or how to sit, stand, and move.
Try not to tuck your backside underneath you, or walk in high-heeled shoes all the time, which thrusts your pelvis out in front and strains your hip flexors and knees. Notice if you bend your knees all the time when you stand or stick your chest out or your chin up. We work a lot with your alignment in MUTU, as it’s truly the foundation of a healthy core and pelvic floor. Read more about alignment and your pelvic floor here.
Think of a hose pipe that gets a kink in it. The water inside is now placed under increased pressure as free flow is prevented. It tries to find ways to escape. Pressure builds up and seeks the weakest point. This is what happens in your body when we move in a ‘kinked’ alignment, and diastasis, hernia, or prolapse may result.
Engage your core correctly
Change the way you go to the toilet!
The Western toilet does not offer a good position for elimination – whilst a full squat is much more functional and comfortable.
We frequently and proudly recommend the Squatty Potty – (mostly for the unicorn 🌈 🦄…and the handsome prince 👑LOL). Recreate a more natural posture by raising your feet to angle your pelvis and pelvic organs to eliminate easily, completely, and without strain. It’ll change your life…. Like, actually.
What about squatting – isn’t that bad for prolapse?
We squat a lot in MUTU – it’s a functional, natural, load-bearing (bone strengthening) and glute-building core exercise. What’s not to love? For a healthy and strong pelvic floor need to prevent prolapse, our glutes need to be strong and sacrum needs to be flexible and hanging in space, not all tucked under you so your pelvic floor muscles are shortened.

To squat correctly, your shins should be vertical, but not tucked underneath, weight through your heels and the outsides of your feet.
Squatting precautions: If you feel bearing down or discomfort in this or any other exercise, STOP and consult with a specialist. MUTU is recommended for prolapse by specialist Physical Therapists. MUTU has video instructions of modifications for all exercises. If you feel any heaviness or discomfort, get advice for your individual circumstances, and don’t squat deeply.
Kegels (how to get them right)
To re-connect and identify the right muscles, you need to isolate and focus on them. On an exhale, try that little squeeze at the front where you wee, then on the next exhale lift the middle – your vagina, then on the next, lift your back passage, imagine drawing your rectum up inside. Don’t clench your butt (this is hard!).
Try these pelvic floor acrobatics a few times to focus on the 3 openings of your pelvic floor and re-connect your brain’s nerve pathways to the muscles. Go front, middle, back… then back again!
Whilst Kegels or traditional pelvic floor squeezes may ‘tighten up’ your pelvic floor muscles in the short term they are simply not enough, and there is a vital element missing in the way these are often performed. The relax phase of any muscle action is every bit as important as the contract phase, and nowhere is this more pertinent than in the case of your pelvic floor. A hypertonic (too tight) pelvic floor is equally as likely to be the problem as a ‘too loose’ pelvic floor. So if when you are Kegel-ing you are doing any of the following: bending your knees, tucking your backside under, or clenching your butt muscles… you’re not actually getting to the deep pelvic floor muscles at all.
Why kegels aren’t enough: The science bit
TL;DR? You need a strong and healthy pelvic floor to help keep your organs inside your body and functioning normally. You need a strong and healthy pelvic floor to prevent leaks and discomfort. But think of your perineum as the ‘trapdoor’. You also need strategies to keep your organs suspended, ‘hoisted up’ where they’re supposed to be. Thats about alignment and pressure. Just squeezing your pelvic floor won’t cut it.
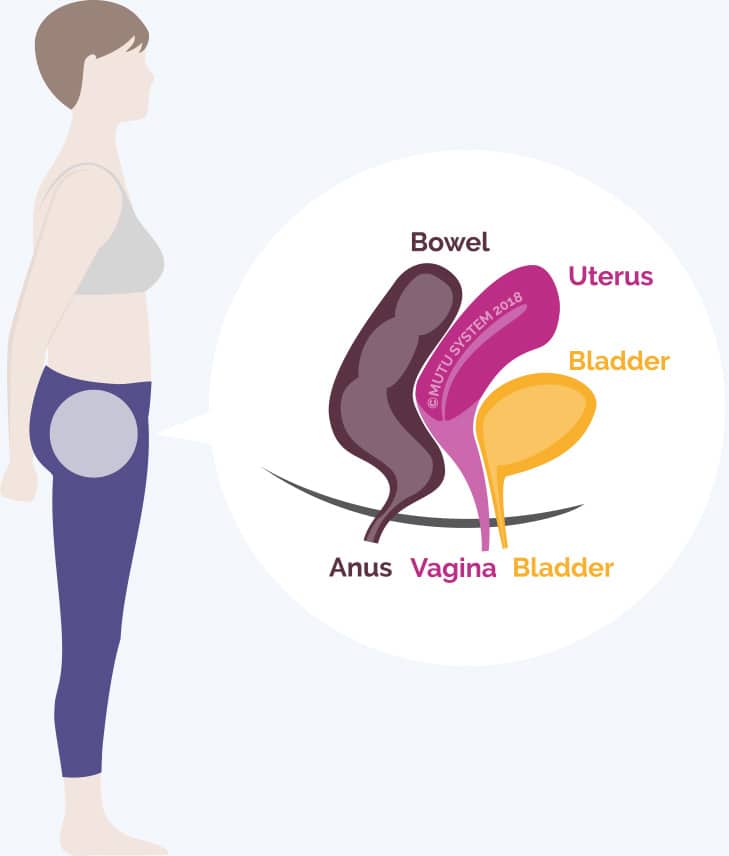
You see it is not only your pelvic floor muscles’ job to ‘hold everything up’ – You have a complex system of fascia and ligaments that hold your organs suspended in their optimal positions inside your pelvis. Think of them as the puppeteer’s strings.
This applies to all the pelvic organs that have their openings at your pelvic floor – your vagina, uterus, bladder and rectum… none of these organs are reliant solely on your pelvic floor to do all the holding work, so, therefore, to focus only on squeezing your undercarriage like crazy can only ever be a band-aid or a temporary distraction from a much more serious problem: that your pelvis is not containing your organs effectively and they are heading south. Pelvic floor exercises are important, but they’re not the whole story.
Of course, your pelvic floor muscles are fundamental to the whole ‘Prolapse’ conversation. They’re integral, forming the undercarriage of the cavity which houses all these organs.
The whole core muscle system is involved
At the top of that cavity is your diaphragm muscle, and the deepest muscle that wraps around the sides is your Transversus Abdominis muscle. At the back are the Multifidus muscles of your spine. Your Transversus Abodminis muscles sit beneath your obliques and run across the sides of your waist. In the middle of your abdomen, you have the Rectus Abodminis muscles also known as the six-pack muscles.
When the intra-abdominal pressure builds or is not contained effectively by the core muscles, due to excessive straining or pushing, poor alignment, aging or a combination of factors, it gets too much. Whilst our bodies won’t actually explode… something still has to give. It might be a hernia popping out at the weakest point, it might be a widening of diastasis recti, or the force may go downwards, pushing and shifting pelvic organs downwards and in severe cases, actually out of our bodies.
That’s Prolapse. When your supportive core muscle, fascia, and ligament structures can no longer hold one or more of these organs in place, they descend. Whilst a ‘weak pelvic floor’ didn’t exactly help the situation, it didn’t single-handedly cause it either.
Further resources for pelvic organ prolapse support
If you suspect you have a prolapse, we recommend you seek one-on-one specialist help from a Women’s Health Physiotherapist / pelvic health PT.
Pelvic Organ Prolapse Support (APOPS)
From Tracy Sher at the Pelvic Guru, The Ultimate Pelvic Anatomy Resource! Links, articles, and videos – this post is kept updated – an amazing resource.
Downloadable (free) PDF information leaflets and diagrams available from the International Urogynecological Association (IUGA) (click ‘Patient Leaflets’)
The Pelvic Partnership | Great resource for pelvic pain in pregnancy.