Clinically Proven, Trusted by Medical Experts, Transforming Pelvic Health
The Evidence-Based Digital Solution Recommended by Healthcare Professionals Globally

Compliance & Accreditation
Meeting Global Healthcare Requirements
US Healthcare Collaborations
Optum Now (United Health Group)
MUTU System is a preferred partner of the Optum Now (UnitedHealth Group) digital health platform, requiring clinical, legal, and technical due diligence. This inclusion enables MUTU to be accessed via one of the largest healthcare and employer benefits ecosystems in the U.S., demonstrating compliance, credibility, and scalability.
US Startup Health
MUTU System was selected to be a part of the prestigious StartUp Health portfolio—an internationally recognized network supporting high-impact digital health innovation. This affiliation validates MUTU’s clinical and commercial potential among investors, healthcare leaders, and payer organizations.
Global Corporate Partnerships
Clinical Evidence
Why NHS Evidence Matters for US Healthcare
MUTU System’s clinical trials and evaluations have been conducted in the UK NHS healthcare system — internationally recognized for rigorous, evidence-based care delivery. These results provide globally transferable credibility, demonstrating real-world impact that meets payer and provider standards.
Peer-Reviewed Research & Clinical Trials
NHS Evaluation Report
Demonstrated measurable value and impact in improving maternal health outcomes across physical and emotional wellbeing.

NHS Clinical Trial
Norfolk & Norwich University Hospital NHS Trust (2022)
Statistically significant improvements in pelvic floor function, abdominal muscle strength, and quality of life.
Clinical Evidence: Outcomes by Symptom
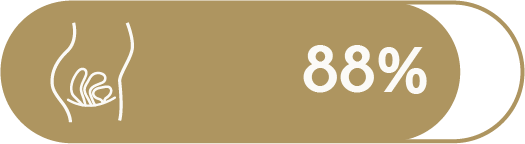
Urinary incontinence

improvement by Week 6 in NHS patients*

Statistically significant symptom reduction***
Confirmed by real-world customer data
of MUTU System users reported improvement in symptoms within 12 weeks**
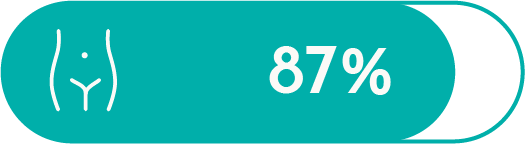
Pelvic Organ Prolapse
of women with prolapse symptoms improved after using MUTU System*
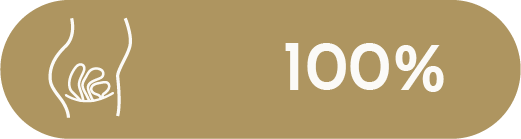
of NHS patients reported improvement by Week 3*
Confirmed by real-world customer data
of MUTU System users reported improvement in symptoms within 12 weeks**
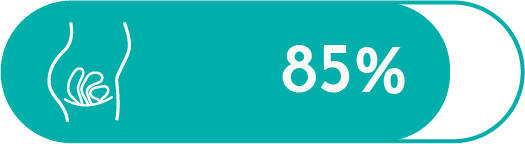
Painful Sex (Dyspareunia)

of women improved painful sex symptoms*
of NHS patients reported improvement by Week 3*
Confirmed by real-world customer data
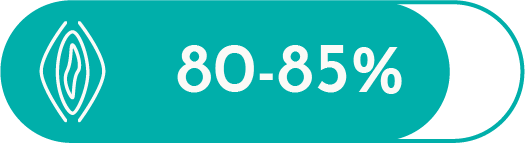
of MUTU System users reported improvement in symptoms within 12 weeks**
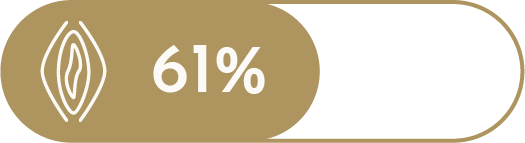
Diastasis Recti

of women reported improvement in abdominal separation*

of NHS patients reported improvement by Week 3*
Confirmed by real-world customer data
of MUTU System users reported improvement in symptoms within 12 weeks**
Maternal Mental Health
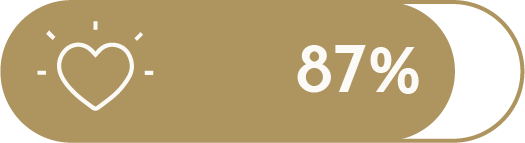
said pelvic health issues affected their mental health*

reported mental health improvement by 12 weeks*

Statistically significant symptom reduction***
Confirmed by real-world customer data

of MUTU System users reported improvement in symptoms within 12 weeks**
Economic Impact for Healthcare Providers
Cost savings
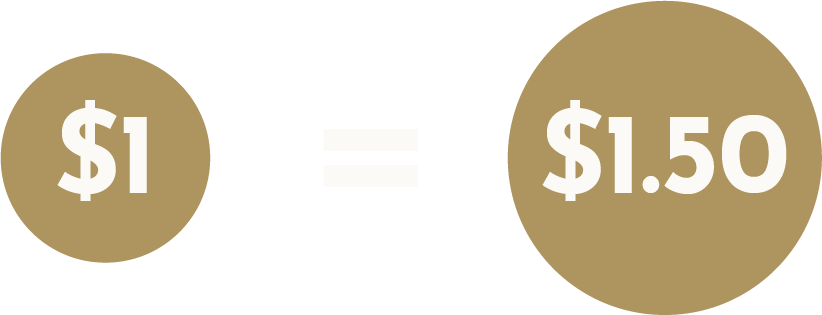
For every $1 invested in
MUTU System…
health plans could see a $1.50 return through reduced maternal health costs.
$1,750-$2,000
Estimated annual savings per member
Estimated savings per member annually by preventing costly urinary incontinence and pelvic organ prolapse procedures.
System-Wide Benefits
Faster rehabilitation
Reduces burden on primary and secondary healthcare services.
Digital delivery
Data source adapted for US audience from UK NHS Evaluation

Patient Voice andHealth Equity Benefits
of NHS physiotherapy patients would recommend MUTU System***
of NHS GP patients would recommend MUTU System***
Patient Feedback
Expert Feedback
Medical Endorsements
Trusted by Physicians, Surgeons & Women’s Health Experts

Dr Jai Seth, Consultant Urological Surgeon
Consultant Urological Surgeon, St George’s University Hospitals NHS Foundation Trust; Founder and Medical Director of the London Bladder Clinic.
“I highly recommend MUTU System where surgery is not required, and also as effective preparation and recovery when bladder surgery might be considered. It is safe and effective and the exercise are evidence-based and shown to deliver significant benefits for many incontinence symptoms” BSc(Hons) MSc MD(Res) FRCS(Urol)

Rachel Craig BSN, RN, CLC, IBCLC
Owner of ‘Hey Mama Rach’ & Maternal/Infant Registered Nurse in the hospital setting
“The MUTU program truly changed my first postpartum experience. I was able to tune into, heal, and fall in love with my body after baby. I believe every mother should experience everything this program has to offer”

Dr Eloise Elphinstone, NHS GP
Specialist interest in women’s health BMS accredited Menopause specialist.
“Having used MUTU myself for both diastasis recti and my pelvic floor, I would very much recommend MUTU as a safe and effective treatment. It is often difficult to know where to start with postnatal and pelvic floor exercises and I found it very easy to follow and flexible with a young baby and as well as enjoyable!”

Dr. Anita Raja, MRCGP, DFSRH, LOC SDI
“As an NHS GP I recommend MUTU because it’s easy to use, only takes 12 minutes a day and it actually works!”

Dr. Phoebe Ajayi, GP and Women’s Health Consultant
“MUTU system a well-rounded and accessible programme that supports women in their postpartum rehabilitation.”

Dr. Ishi Bains – GP, Clinical Director, Specialist interest in Women’s Health
“As a busy working mum who’s self care is often low on the list of priorities MUTU made it easy, doable and enjoyable to recover postnatally as well as providing a supportive realistic way of getting back into exercise.”

Dr. Katy Chisenga, GP
“As a doctor and a new mum, I found the postnatal recovery journey overwhelming—there was so much conflicting advice, and I wasn’t sure where to begin. MUTU is a game changer for new mums: everything you need in one place makes it much easier to focus on physical and mental healing, even in the fog of mum brain and newborn chaos.”

Dr. Kimya Tarr
“Dr. Kimya Tarr is an experienced NHS General Practitioner (GP) and Medical Lead at Quadrivia.ai, where she combines her clinical expertise with a passion for digital health transformation and the integration of artificial intelligence (AI) into healthcare. With nearly a decade of experience as a GP and over seven years in digital health, Dr. Tarr is dedicated to improving patient care through innovation and technology.”

Dr. Odinaka Nwodo, MBChB, MRCSEd, MRCGP
NHS GP, Urology clinican and primary care
“The MUTU programme has impacted the lives of so many women in my practice. I am glad that the NHS have clearly identified the value in MUTU’s transformational programme.” Dr Odinake Nwodo MBChB, MRCSEd, MRCGP

Dr Raj Arora, GP
NHS GP and Health Educator.
“I personally used the MUTU System program with great results for my diastasis recti, back pain and pelvic floor. I recommend MUTU to my patients.”

Dr. Tracy Sher PT, DPT, CSCS
Owner and Clinical Director, Sher Pelvic Health and Healing in Orlando FL; CEO, Pelvic Global
“MUTU System is a global leader in safe pelvic floor and core programming and a robust client experience. Much more than simply an online exercise program.”
How MUTU stands apart
MUTU System is the only digital postpartum solution offering a unique blend of clinical credibility, healthcare partnerships, and patient engagement.
Compared to general fitness or pelvic floor digital app solutions, MUTU delivers:
- Clinical Evidence: Peer-reviewed studies, NHS trials, and independent evaluations.
- Institutional Trust: Adopted by healthcare systems and reviewed by clinicians.
- Compliance Standards: Meets HIPAA, GDPR, DTAC, ORCHA bench marks.
- Medical Endorsement: Backed by OB-GYNs, pelvic health experts, and primary care physicians.
- Accessibility & Equity: Designed to be sacalable for diverse populations and social determinants of health.
This positions MUTU as a medically truested, outcomes-driven solution unmatched in its class.
- Trusted and implemented by healthcare systems
- High user adherence and satisfaction
- Meets rigorous digital health compliance standards
- Supported by respected medical experts and clinicians
Interested in bringing MUTU to your members or patients?
FAQs for healthcare professionals
You can refer to try MUTU directly via our website. When signing up they will get a free trial before purchase is completed. If you’re looking to procure or commission MUTU for your hospital, clinics or healthcare system, please contact us.
The MUTU System program aligns with the IRS definition of “medical care” (IRC Section 213(d)) and qualifies as a reimbursable expense (with LMN) when used to:
- Treat postpartum conditions such as diastasis recti, incontinence, pelvic organ prolapse, and pelvic floor dysfunction
- Provide preventative care for long-term musculoskeletal health after pregnancy
- Improve the structure and function of the body, specifically core and pelvic floor strength
More information and downloadable Letter of Medical Necessity here.
To discuss healthcare provider partnerships with MUTU, discuss research or data, and to direct your patients and clients to MUTU, please contact us.
To discuss working with us as an Ambassador, please get in touch with Wendy, NIA Fellow and Director at MUTU.
Data protection and clinical safety are managed by Naq Cyber. See our Privacy Policy here.
Data sources
* MUTU NHS Clinical Trial View source >
** Findings confirmed by real-world customer data (n=12,000+). Self-reported outcomes are based on surveys completed by MUTU System users at 3, 6, and 12 weeks during the program (2021-2025) View source >
*** NHS Evaluation of MUTU View source >