Our pelvic floor helps us stay dry until we get to a bathroom, holds us stable and strong, allows us to jump, laugh or sneeze without leaking, gives us orgasms and maybe it births our babies. It’s BUSY.
So pelvic floor connection, awareness and strengthening is a habit worth cultivating.
Brushing our teeth, washing our face, drinking water to hydrate, maybe taking a multivitamin.… we do these every day to maintain our wellbeing and because we know they do us good. Taking care of your pelvic floor is kinda the same.
This free resource will help you get to know your pelvic floor better.
We’ve included information and links to pelvic floor exercises, tips for self care, methods for strengthening (and relaxing!) your pelvic floor and a ton of other pelvic floor related knowledge to help you on your postpartum care journey.
How to improve bladder leaks and incontinence after giving birth
Bladder leaks or Incontinence are common – you are not alone 💜 But you CAN improve it, so read on!
Wherever you are on your journey, whether you’re in your twenties, thirties, forties, fifties or beyond. First time pregnant, new mom, or not-at-all-new Mom, perimenopausal or anywhere else, your pelvic floor needs strategies to avoid those bladder leaks and incontinence.
Women’s bodies are always evolving, changing, always kinetic, never static. Throughout our monthly cycles, pregnancies and our lives, hormones are shifting, our bodies need to move, stretch and work for us.
What is your pelvic floor?
When we talk about the pelvic floor, we’re talking about the muscles and tissues around your pelvis.
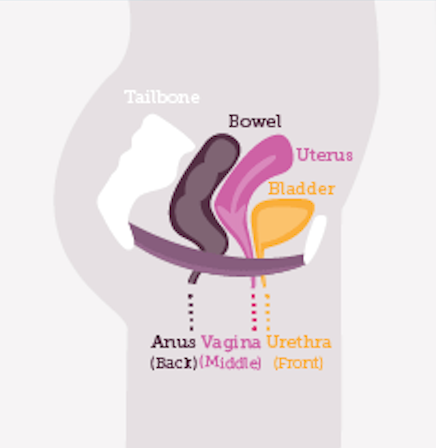
Your pelvic floor muscles support organs like your large intestines (bowels), bladder, and internal reproductive organs.
They attach at the front and at the back — from pubic bone to tailbone — sort of like a hammock.
How do the Pelvic Floor Muscles Work?
Your pelvic floor muscles need to be simultaneously strong, flexible, and functional.
This means they need to be able to be fully relaxed as well as contracted as required. Too tight or too loose can make for a pelvic floor that doesn’t work optimally.
We learn to control the pelvic floor muscles early in life
For the most part, we learn how to control our pelvic floor muscles early on in life when we learn how to control when we pee and poop.
These movements become routine pretty quick. This means that we’re often engaging our pelvic floor muscles without thinking about it.
Our pelvic floor muscles are also partially responsible for reaching orgasm. This is often done without specifically thinking about using these muscles.
Why Does Pelvic Floor Health Matter?
It can be easy to take pelvic floor health for granted until there’s an issue.
Your pelvic floor muscles are important for holding things together and letting things go. It’s a stabilising force for your organs and spine, protecting both from external stressors.
Issues with this muscle group are often more significant than we give credit:
- Almost 1 in 4 women between the ages of 18 and 44 experience incontinence.
- 30% said pelvic health affected their performance or focus at work
- 36% felt anxious and embarrassed in the workplace due to pelvic health issues
- 87% of women said that dealing with pelvic health issues had affected their mental health at some stage

How Pelvic Floor Health Can Affect Your Bladder, Bowels and Sexual Function
These muscles are both supportive and flexible, allowing for waste to be removed from your body in a smooth and controlled way.
Holding in your pee or poo often or for long stretches of time can both make it more likely to cause pelvic floor issues.
Feeling like you can’t void properly can also be a symptom of underlying pelvic floor dysfunction.
You could be at increased risk of infection, inflammation, and digestive issues because of this.
It can also matter when it comes to enjoying sex and having an orgasm, too. This is true for people with penises or vaginas and for penetrative and non-penetrative sex.
Pelvic floor health matters in pregnancy, birth, and postpartum in many ways.
What is pelvic floor dysfunction?
Pelvic floor dysfunction (or disorders) is a group of conditions that can occur when the correct functioning of a woman’s pelvic organs are compromised.
It mostly occurs when the muscles or connective tissues are weakened, injured, stretched or too tight.
This can in turn lead to bladder control issues, bowel control issues or pelvic organ prolapse (where the organs in the pelvis drop).
How common is pelvic floor dysfunction?
Pelvic floor dysfunctions are extremely common for women.
According to University of Chicago Medicine, a minimum of 1 in 3 women will experience one in their lifetime, with 1 in 4 women older than 20 suffering from symptoms like incontinence, urine or stool leakage.
If you’re experiencing this yourself or just generally worrying about your pelvic floor health – remember you’re not alone and this is very, very common.
There’s also many things you can start to do today to begin improving things.
Do you need surgery to fix a pelvic floor dysfunction?
According to stats, one in five women in the will need to undergo surgery to treat a pelvic floor disorder.
The good news is in many cases you can manage symptoms and avoid surgery or further issues, by simply changing some of your movement (and bowel movement) habits.
Non-surgical solutions include:
- Pelvic floor exercises
- Subtle adjustments in the way you sit and go to the toilet
- Untucking your tailbone
- Looking after your gut health
- And even changing the footwear you use (goodbye high heels!).
For some women a vaginal pessary can be a good option if you cannot have, or would prefer not to have, surgery.
But when should you get surgery?
The answer to this is when:
- Symptoms bother you enough that you want it fixed
- Pelvic floor rehab, toileting / alignment strategies and non-surgical options like a pessary… have not improved matters.
Mesh surgery for prolapse can be effective but is not without problems or controversy.
What are the Symptoms of a Weak Pelvic Floor?
There are many symptoms connected with a weak pelvic floor.
If you are experiencing any of these you may have pelvic floor issues that need attention:
- Leaking urine when you workout, bounce, laugh, cough, run, or sneeze
- Needing to pee frequently
- Less vaginal sensation or painful vaginal sensations
- Painful sex or reduced sensation during sex
- Pelvic organ prolapse (POP)
- Bowel dysfunction, including difficulty pooping and anal incontinence (AI)
- Hypertonic Pelvic Floor Disorder (this is when your pelvic floor is too tight)
What does a weak pelvic floor feel like?
The way a weak pelvic floor “feels” will vary from person to person. Not everyone with a weak pelvic floor will experience the same sensations!
That being said, here are some common descriptions of what it may “feel” like for individuals with a weak pelvic floor:
- Sensation of pressure or heaviness: Many people with a weak pelvic floor describe a constant or intermittent sensation of pressure or heaviness in the pelvic area. It can feel like there’s something weighing down in your lower tummy or a dragging discomfort inside your vagina.
- Lack of control: Many women can feel a lack of control over their pelvic muscles. This can manifest as difficulty holding in gas or stool, or feeling like they can’t stop the flow of their pee when they need to.
- Sudden urges: There may be a frequent and sudden urge to pee, which can be hard to control. This can lead to rushing to the bathroom or experiencing leakage before reaching the toilet.
- Discomfort or pain: Pelvic pain or discomfort, which can range from mild to severe, is a common feeling for women with a weak pelvic floor. This can feel worse during physical activities or while sitting for a long time.
- Sensation of “Dropping”: Some women with pelvic organ prolapse, which can result from a weak pelvic floor, describe a feeling of organs (such as the bladder or uterus) coming down into the vagina. This can create a noticeable sensation of something “dropping.”
- Sexual discomfort: For some women, sex can be uncomfortable or painful due to the weakened pelvic floor muscles. This can lead to feelings of frustration or anxiety related to intimacy.
- Incomplete emptying: Women may constantly feel like they haven’t completely emptied their bladder or bowels. This can be irritating and lead to repeated trips to the toilet.
What causes a weak pelvic floor?
Like most things in our bodies, biomechanics and alignment, excess strain, trauma, genetics, major changes in your health, surgery, substantial weight gain, age, and injury can all contribute to pelvic floor dysfunction.
Believe it or not, your mental health and habits can factor into the strength of your pelvic floor, too.
Learn more about the links between pelvic floor health and mental health here.
Does Having a Baby Weaken Your Pelvic Floor?
Yes, having a baby can definitely contribute to the weakening of the pelvic floor muscles in some women.
Your body is normally doing quite a bit of heavy lifting to maintain proper organ placement and function in our pelvic brim even without adding the massive changes of pregnancy into the mix.
As your uterus does its incredible expansion and you grow a whole bitty human in there (or a few of them at once), it is obviously going to put some added strain on your pelvic muscles and ligaments!
Secondly, there is a whole soup of hormones in there to help bend, stretch, and soften the muscles and ligaments in your pelvic brim.
It’s a very efficient and wonderful thing to happen to help make space for and move your baby out of your body.
The downside of this is that it’s not always the smoothest dance or one that ‘bounces back’ in weeks after being so changed for many months.
It’s usually an assortment of several reasons rather than just one
There are loads of reasons (and usually some assortment of several) that can make for a weaker pelvic floor in pregnancy and postpartum.
Some of these come from the normal changes occurring in pregnancy which happen to affect some mums more than others.
Other reasons are due to circumstances that arise in the process of giving birth or from certain birthing procedures.
How Do You Tell If Your Pelvic Floor is weak?
Our pelvic floor is tucked away out of sight, making it tricky to assess its condition by ourselves.
However, knowing the signs that signal a not-so-strong pelvic floor can be your secret weapon in getting the help you need ASAP.
Little signs your body might be sending you:
- Experiencing unintended urine leaks.
- Finding it challenging to reach the restroom in time.
- Dealing with discomfort or pain in the pelvic region.
- Noticing a decrease in sensation during sexual activity.
- Accidentally letting out gas in an unexpected moment.
For a professional diagnosis, you must see your healthcare provider.
Your doctor will chat with you about your medical history and listen to what’s been bothering you.
They’ll also give you a once-over to see if there are any muscle spasms or knots causing trouble, and check for muscle weakness.
Depending on your situation they may carry out an internal exam or potentially use electrodes to see how well your pelvic muscles are working.
When should I see someone if I’m experiencing Pelvic Floor pain?
Your first port of call should be a Pelvic Floor Physical Therapist (US) or Women’s Health Physio (UK).
It’s important to first rule out a possible infection or chronic inflammatory condition. This is usually done with some simple tests.
If your pelvic pain is persistent and you’re sure it’s not an infection, you may be referred to your GP, midwife, or OBGYN about your pain.
They may recommend having you go for additional testing or refer you to a specialist.
Depending on your level of pain, they may suggest starting with some of the exercises and mental health practices first and have you follow up.
If it is available in your area, with your insurance or finances, and seems interesting to you to do, you might want to make an appointment with a pelvic floor therapist.